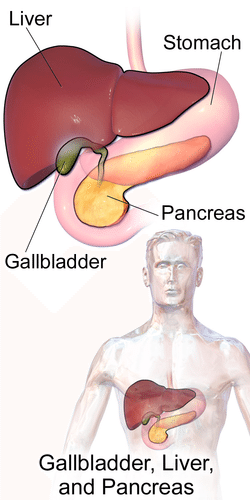
 The treatments of chronic liver disease have improved dramatically over the past 10 years with new, potent and effective therapies available for conditions such as hepatitis B and C and soon to be available for primary biliary cholangitis and fatty liver disease. These treatment advances have highlighted the need for safe, effective and patient-accepted methods of assessing disease prognosis.
The treatments of chronic liver disease have improved dramatically over the past 10 years with new, potent and effective therapies available for conditions such as hepatitis B and C and soon to be available for primary biliary cholangitis and fatty liver disease. These treatment advances have highlighted the need for safe, effective and patient-accepted methods of assessing disease prognosis.
The prognosis of chronic liver disease has historically been determined by the degree of fibrosis or scarring within the liver and this has not changed as treatments have advanced. Therefore, it is more important than ever to assess the degree of scarring in all patients with liver disease, regardless of cause, and to be able to do that serially over time.
There are currently three methods to assess how much fibrosis is present within the liver. These are serum biomarkers or blood tests, liver biopsy or transient elastography.
Blood tests are the most widely available method to estimate fibrosis. There are several available commercial tests and several simple formulas that clinicians can use to estimate the amount of fibrosis. All of these tests share similar characteristics. They are relatively inexpensive, non-invasive and excellent at predicting minimal fibrosis or advanced cirrhosis. They are of little use when patients are not at either end of the fibrosis spectrum. Therefore, the use of these tests as the sole method to determine fibrosis stage should be discouraged.
Liver biopsy has been the gold standard for assessing fibrosis. Unfortunately, the reputation of a liver biopsy has taken a beating as it is invasive and potentially associated with complications such as pain, bleeding, etc. Liver biopsy actually has multiple purposes in assessing patients with liver disease. It is performed to help determine the etiology of the liver disease, and to evaluate the extent of inflammation, fibrosis and fatty infiltration. In many circumstances, liver biopsy remains a very important tool in the evaluation of liver disease and should be continued to be used in those specific settings.
Transient elastography is the third and newest method to determine how much fibrosis is present in a diseased liver. This technology employs ultrasound technology which measures the velocity of a shear wave after the wave has bounced off the liver and returned to the transducer. This technology is very attractive as it is relatively inexpensive, is non-invasive and can be repeated serially thus giving the patient a way of tracking disease progression or improvement over time. The test takes about 10 minutes and results are immediately available.
While this sounds wonderful and it is, there remain several drawbacks to this technology. Results are affected by eating so patients need to have had nothing to eat for several hours prior to the test. The test is excellent at differentiating mild disease from advanced disease but is not as effective in differentiating moderate disease from either extreme. In addition, results may be variable in patients with a high body mass index and the results are highly dependent upon the skill of the person performing the test. Despite these negatives, transient elastography is a very promising tool to assess all patients with liver disease and further advances in this technology are forthcoming.
It is highly likely that the assessment of fibrosis in the future will be a combination of the above modalities, with the most likely combination being blood tests and transient elastography as these tests are the least expensive, least invasive and most accepted by patients.
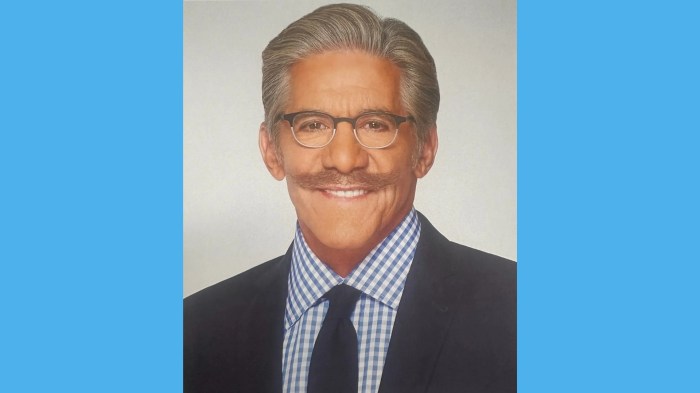
David Bernstein, MD, is chief of gastroenterology, hepatology and nutrition at North Shore University Hospital and Long Island Jewish Medical Center.