Researchers on Long Island are looking at whether the body’s own immune system’s overreaction can be leading to the most severe COVID-19 cases, which could open the door to different treatments.
Northwell Health, Cold Spring Harbor Laboratory and nine other medical research institutions are studying whether an overreaction by white blood cells may cause the most severe cases of coronavirus, potentially leading to additional treatments.
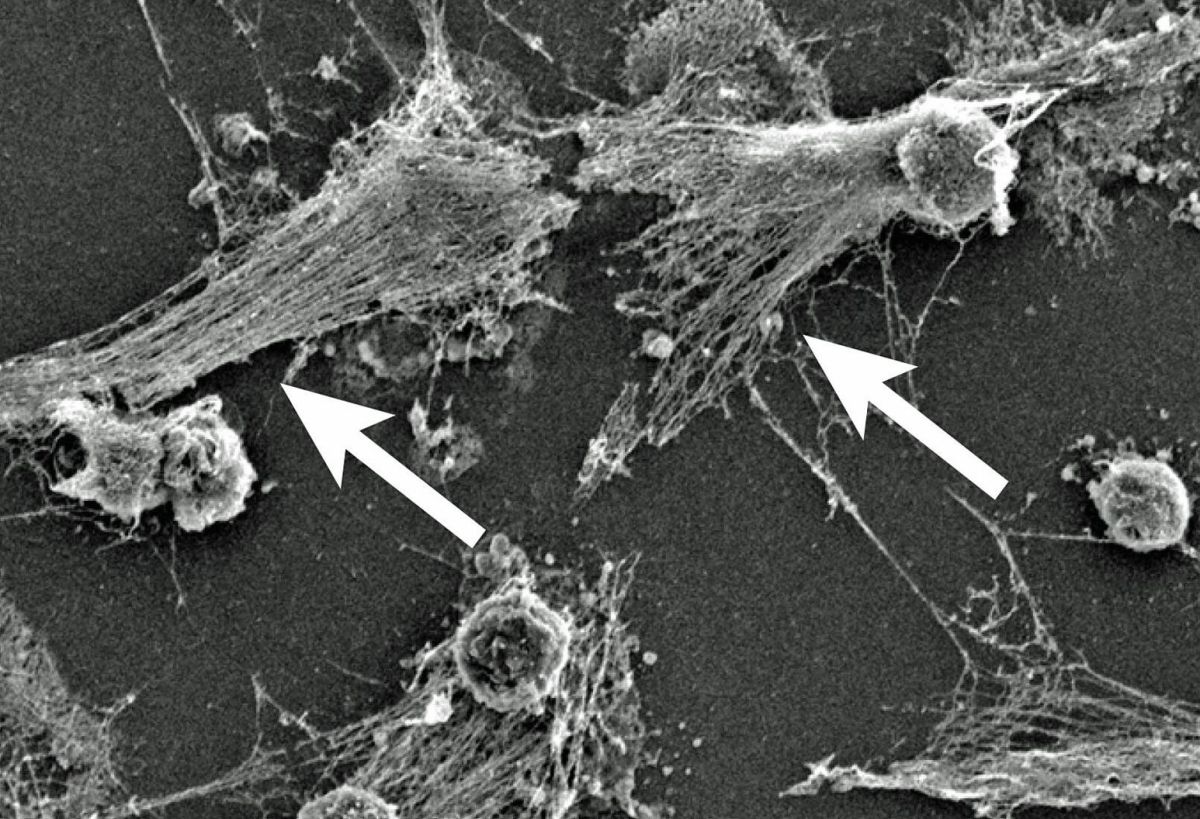
The researchers are looking at whether “overactive immune cells” produce Neutrophil Extracellular Traps or NETs, which may be responsible for the most severe cases.
The group of institutions, known as the NETwork, on Long Island includes Cold Spring Harbor Laboratory, Northwell’s Feinstein Institutes for Medical Research and the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell.
A paper published last week in the Journal of Experimental Medicine concluded that patients with COVID-19 infection sometimes develop Acute Respiratory Distress Syndrome or ARDS, pulmonary inflammation, thick mucus secretions in the airways, extensive lung damage and blood clots.
“This late stage of the disease is difficult to manage,” according to Northwell. “In the worst cases, patients require invasive mechanical ventilation, and still, a large number of patients die.”
This condition, however, may result from overactive white blood cells or neutrophils that, in the body’s effort to battle the infection, can damage lungs and other organs.
“We propose that excess NETs may play a major role in the disease,” said Betsy Barnes, lead author of the paper and professor at the Feinstein Institutes. “It will be important to determine whether the presence of NETs associates with disease severity and/or particular clinical characteristics of COVID-19.”
NETs can lead to mucus in cystic fibrosis patients’ airways and acute respiratory distress syndrome or ARDS in flu or influenza.
If findings show excess NETs cause severe symptoms of COVID-19, Northwell said a new “avenue of treatments may be deployed to help COVID-19 patients,” reducing the need for intubation.