Many hospitals on Long Island were inundated with Covid-positive patients after the pandemic hit the region in March. Of those health care heroes who answered the call — putting their own lives at risk to help others — a handful stood out from the pack as winners of the 2020 Bethpage Best of Long Island contest.
The winners include Stony Brook University Hospital, which won the title of Best Hospital on Long Island; NYU Langone Hospital—Long Island in Mineola, which won Best Maternity Ward on Long Island, and ProHEALTH Urgent Care, which won Best Urgent Care.
Each of these establishments exhibited an extraordinary response to Covid from the get-go and their medical and professional staff proved their remarkable skills, strength, and character. Health care practitioners rose to the daunting occasion and used both their interpersonal and professional skills not only to save lives but to touch lives. So, what defines a health care hero? Read on to see what these standout facilities and their first-rate staff have in common.
Health care heroes agree that combatting Covid-19 requires a collaborative effort not just for the health of their patients but for each other’s emotional wellbeing, too.
BEST HOSPITAL
Stony Brook University Hospital Leads Patients and Staff Through the Storm
Stony Brook University Hospital was quick to respond to the needs of the community, and all hospital staff—physicians and nurses, radiology, and housekeeping—united to assure that each patient had their best chance at recovery and that colleagues felt supported in the process.
Spearheading efforts to increase capacity at Stony Brook’s Intensive Care Unit (ICU) was James Vosswinkel, MD. MD, FACS; Chief, Trauma, Emergency Surgery and Surgical Critical Care; Medical director, Trauma Center, and Surgical ICU, Stony Brook Medicine
Stony Brook’s medical team collaborated with other health care professionals on a local, nationwide, and international level, Dr. Vosswinkel said. Hospital departments worked to ensure they had an adequate supply of oxygen, ventilators and other respiratory supplies, PPE and more.
“We were a really well-oiled machine where each department put their best foot forward and was integrated at a very high level together to truly address the pandemic,” the doctor said.
Stony Brook tripled their entire ICU capacity in an effective, safe fashion.
“We provided patients with the best that modern medicine could offer to try to get them to recover,” he added.
“We came together and really supported one another and worked together toward a common goal of keeping each other safe but also doing the best we possibly could do for our patients,” said Dawn Teer, RRT, NPS, CPFT, a respiratory therapist at Stony Brook University Hospital.
Teer was a lead therapist and staff supervisor at the height of the pandemic. She also took regular assignments, making herself available and present to patients and staff as much as possible. Teer recalled a young patient who was intubated for months and came very close to losing his battle more than once.
“We never gave up on him,” she said. “We kept trying different kinds of ventilator strategies, we wouldn’t give up and he wound up coming off and living.”
Strong leadership offered staff and patients the support needed to get them through a most challenging time. Sofia Marie Reyes, staff and relief charge nurse at Stony Brook, assumed responsibility as a relief charge nurse in the first pop-up Covid Intensive Care Unit at Stony Brook University Hospital. Reyes was responsible for training other nurses from non-ICU units who had little to no experience in an ICU. Some of the nurses hadn’t stepped foot on a critical care unit in up to 15 years if at all—and they were understandably initially intimidated, recalls Reyes.
“I wanted to help alleviate their fears. I couldn’t imagine what they were going through—dealing with the machines and the ventilators, the IV pumps, and just how sick these patients were,” Reyes said.
She took the time to get to know her staff, learn all of their names and get them to a place of confidence. She patiently explained to them how to run an IV, administer medications and use the ventilators. Reyes said she was able to lead by example due to the tremendous collaboration and support from all at Stony Brook.
“I feel that my Covid ICU had strong teamwork between the MICU and PACU nurses, MICU attendings and fellows, the respiratory therapists, and the ancillary staff, clerks and nursing assistants,’ she added. “I had—still have—an amazing and supportive nursing leadership—my nurse manager and clinicians—who assured we had adequate PPE and as much staffing and resource supplies as we could get.”

BEST URGENT CARE CENTER
ProHEALTH Urgent Care Heals and Educates
ProHEALTH Urgent Care’s Long Island facilities were exemplary in meeting their patients’ needs safely and effectively.
“The onset of the Covid-19 pandemic changed medicine for the urgent care clinicians,” recalled Kevin Patel, PA, of ProHEALTH Urgent Care in Jericho. “At its peak, the hospitals were at maximum capacity and general clinicians were unable to care for patients in an outpatient setting. We were overwhelmed with high volumes daily throughout the months of March, April, and May.”
The facility received support from providers from different departments of ProHEALTH.
“It became a group effort to make sure the community was tested and contact tracing was done by the department of health to stop the transmission and lower the rate of infection,” Patel said.
Patients were doing everything they could to avoid a trip to the emergency room and ProHEALTH medical staff were doing everything they could to support those patients who would otherwise have taken their symptoms to the hospital.
“It became our jobs to make sure these patients got the best care necessary,” Patel said.
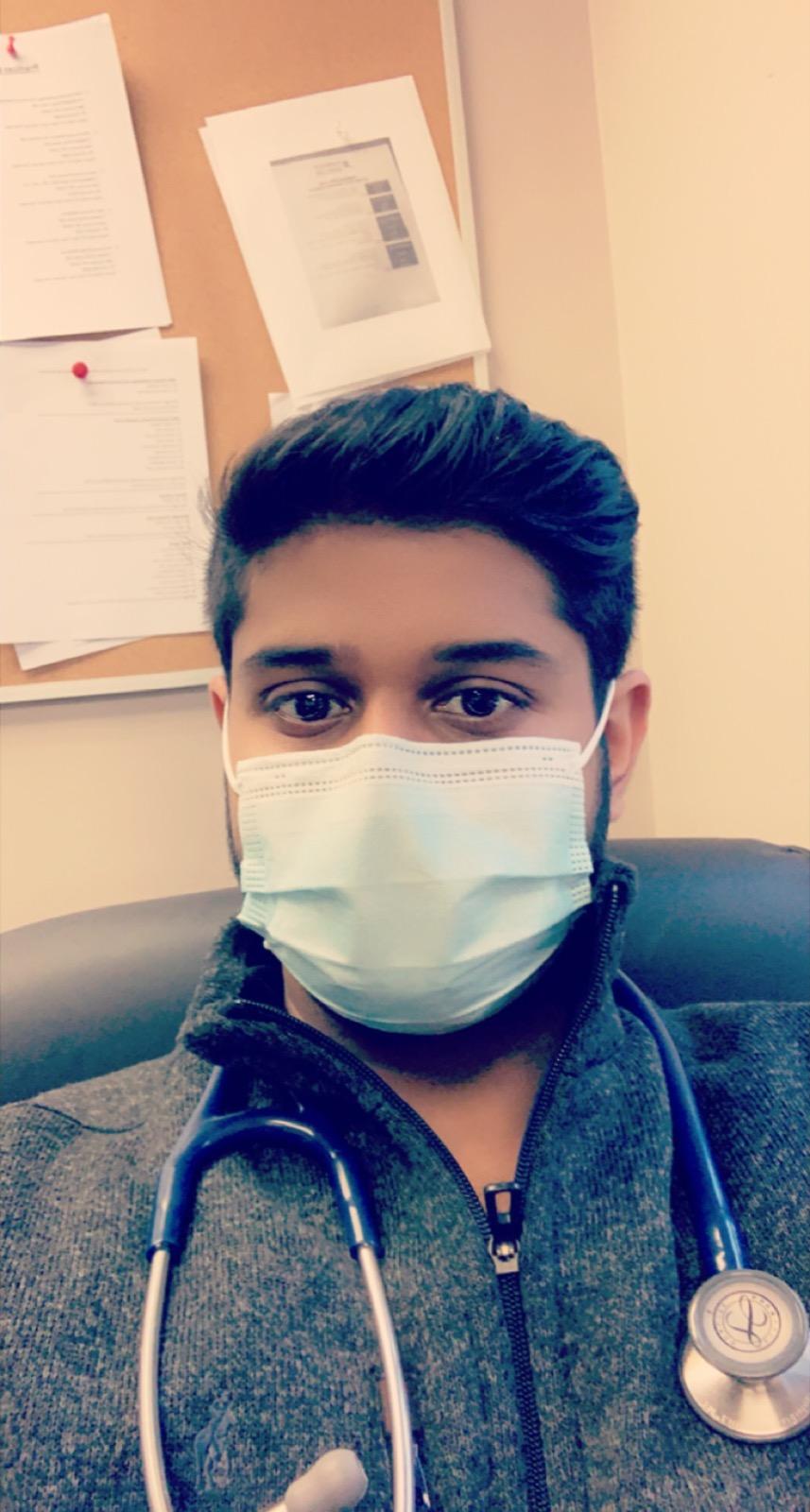
“We developed a very effective system for evaluating Covid patients in a safe manner,” said Diane Peterman, MD, of ProHEALTH West Islip Pediatric Urgent Care. At the pandemic’s peak, patients were treated in their cars. Dr. Peterman says, “We were able to obtain vital signs, test and evaluate individuals without exposing them to other ill patients. The entire staff remained positive, professional and cohesive while maintaining a safe environment. We were very fortunate to receive support from our fellow colleagues from other departments. It was a unique opportunity to work with a wide variety of specialty groups who offered their time.”
Patient education was also a priority, noted Dr. Peterman.
“I would prescribe supportive medications such as inhalers, nebulizers, supplements and encourage patients to take time to exercise and get fresh air and sunshine,” she said.
Staff also distributed educational and instructional packets with updated information on Covid.
At a time of great fear and uncertainty, “We provided a sense of relief in the community because many of the patients did not understand how to process major changes in their daily life activities,” added Patel.

BEST MATERNITY WARD
NYU Langone Hospital Preserves the Miracle of Childbirth
Healthcare heroes at NYU Langone Hospital—Long Island also saw their responsibilities change practically overnight, particularly in Labor and Delivery.
During the height of the pandemic, Catherine Bell, a nurse manager in L & D, led her team in the care of acute, adult Covid patients when one side of the mother/baby unit was converted to an adult unit. She also managed the other half of the unit with moms and babies. Bell says that the patients in L & D/maternity units are typically healthy women of childbearing age, hence the nursing responsibilities and experiences were also drastically different than in other areas pre-Covid.
“Our population of patients is very unique,” she said. “They are healthy—they had a baby, they have needs, and we have to take care of them—but they are not sick. It is a very different type of nursing than that of other nurses in other areas.”
Nurses were confronted with horrific experiences that most of them had never encountered, Bell said.
“I have been doing mother-baby maternity, labor and delivery for 36 years,” she said. “That’s all I know.”
Bell added that most of the nurses she worked with share similar work histories. The night that her unit was converted was one she will never forget. Bell received a phone call from a nurse at 12:30 a.m. one morning in March.
“The nurse said ‘Cathy, it’s happening,’” she recalled. “It went from zero population to every room was full. Within hours, I went from talking about breasts, lactating, and breastfeeding to, ‘Wait, how old is this woman? She’s 92.’”
Bell recalls having conversations with patients in one moment and then suddenly needing to call rapid response, thinking they had to be intubated. Within a few days of the conversion, “we had our first death,” Bell said. To a unit of labor and delivery/maternity nurses, the entire experience was “shocking,” Bell said.
“Our unit is primarily a happy place,” she said. “We have the babies. We have the moms.”
Bell said she and the other nurses stood strong and carried their patients and each other through the process. She assured her staff she was right there with them and that they could count on her to work alongside them. For her L & D patients, she and the other nurses worked wholeheartedly and truly were amazing in helping to maintain a sense of normalcy for an optimal and special birth experience in spite of all the changes and looming fear in the hospital.

“Every day, we learned something new,” said Christine Boyd, registered nurse. “We had to stay on top of everything. If mom was positive, the baby went to the pediatric floor and the mom would stay in the hospital. We were discharging after 24 hours after delivery, 48 hours for a c-section.”
Most mothers, if cleared, couldn’t wait to go home.
“There were sick moms and there were moms that got vented,” Boyd said. “We tested every single mother right when they came in.”
Hospital staff are still testing, Boyd noted.
“It was a different way of doing the delivery with the couple but we made it work,” Boyd said, adding that for husbands or other support persons that could not be present in the delivery room, they’d FaceTime.
Patients were scared. Boyd says nurses provided additional comfort and support to ease their fears.
“That moment your child being born-you can’t get that back, and I didn’t want it to be panic,” she said. “We didn’t want them to lose out on a most memorable experience.”
Boyd recalled one patient who was on a ventilator when her baby was delivered preterm.
“It was very hard to think, ‘Was she going to wake up and see her child? Was the child going to see her mother?’” Thankfully, this family’s story had a happy ending,” said Boyd. About one week following the baby’s birth, “they brought me to the NICU when the mom was holding the baby and I got to be there when she was discharged home.”
Boyd was overwhelmed with joy.
“I was just so happy, I started to cry happy tears,” she recalled. “To see her awake and holding her baby was pretty amazing and I know it was the work of the entire hospital from the NICU staff to the ICU staff to the residents, the attendings, anastasis—everybody.”
Health care heroes agree that It was these types of success stories, the support of their respective medical care institutions, as well as the outpour of community support that helped them persevere and do their jobs. Gratitude was felt everywhere, Boyd recalled.
“We could feel the support of the community on the outside, too,” she said. “There were people with signs thanking us and it was so appreciated to have that support.”